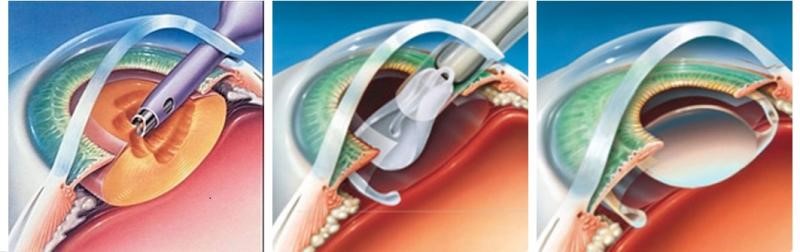
Cataracts is a condition where the lens of your eye becomes cloudy. Your vision becomes hazy, darker, and less colourful. You may also experience vision loss. Cataracts are usually caused by aging, and may become more common around the age of 50. Cataracts can also be caused by trauma to your eye or diabetes.
Aging and exposure to sunlight can cause cataracts. Changes in your eyes are often a normal part of aging. But the changes do not always lead to cataracts. Cataracts can also happen after an eye injury, as a result of eye disease, after you use certain medicines, or as a result of health problems such as diabetes. Sometimes children are born with cataracts.

Whether you need cataract surgery depends on how much of a problem the cataract causes for daily activities like driving and reading. Surgery is almost always by your choice (elective) and can be scheduled when it is convenient. For people who decide to have surgery, the surgery usually works very well.
Some people have to have surgery. Children are sometimes born with cataracts that need to be removed. Other people may get cataracts after an eye injury or as a result of eye disease or other health problems. Cataracts from these causes may also need to be removed.
Conductive Keratoplasty (CK) is a non-invasive procedure which utilizes radiofrequency energy to correct presbyopia and low hyperopia with or without astigmatism. It can also be used to correct residual refractive error after laser in-situ keratomileusis (LASIK) or cataract surgery. The portable nature of CK and its low comparative cost make it an important tool in the ever-evolving world of refractive surgery.
Other procedures used to correct hyperopia include LASIK, photorefractive keratectomy (PRK), noncontact and contact laser thermal keratoplasty (LTK), diode laser keratoplasty, thermos keratoplasty, intracorneal implants, and intraocular lenses. While LASIK is the most popular technique for surgical correction of low to moderate hyperopia, and PRK and laser-assisted sub epithelial keratectomy (LASEK) are most popular for low hyperopic errors, some patients are not good candidates for laser procedures due to anatomical, pathological, or psychological reasons. For these patients, CK involves no laser, change to the central cornea, tissue cutting, or tissue removal. Several studies have shown that CK is an effective, predictable, stable, and safe procedure.
A cornea transplant replaces diseased or scarred corneal tissue with healthy tissue from an organ donor.
There are two main types of corneal transplants: traditional, full thickness cornea transplant (also known as penetrating keratoplasty, or PK) and back layer cornea transplant (also known as endothelial keratoplasty, or EK).
A graft replaces central corneal tissue, damaged due to disease or eye injury, with healthy corneal tissue donated from a local eye bank. An unhealthy cornea affects your vision by scattering or distorting light and causing glare and blurred vision. A cornea transplant may be necessary to restore your functional vision.
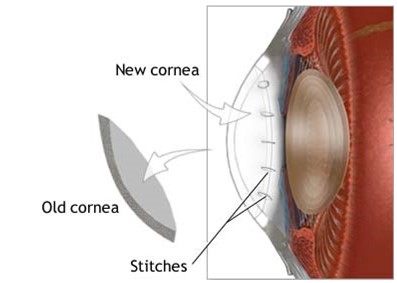
A healthy, clear cornea is essential for good vision. If your cornea is damaged due to eye disease or eye injury, it can become swollen, scarred or severely misshapen and distort your vision.
A corneal transplant might be required in cases of conditions such as trichiasis, where eyelashes turn inward and rub against the surface of the eye, causing scarring and vision loss.
A cornea transplant may be necessary if eyeglasses or contact lenses can’t restore your functional vision, or if painful swelling can’t be relieved by medications or special contact lenses.
Certain conditions can affect the clarity of your cornea and put you at greater risk of corneal failure. These include:
Surgery reduces the pressure in the eyes by opening blocked drainage angles or creating a new opening that fluid can flow through to leave the eye. In some cases, surgery may be done to relieve pain caused by glaucoma.
Medicine will usually be tried before surgery is considered. Doctors can use either a surgical cutting tool or a very focused beam of light, called a laser, to do surgery for glaucoma. Laser surgery is usually the first type of surgery tried. If laser surgery doesn’t help, your doctor may try conventional surgery.
Surgery choices for adults-There are three basic types of surgery for glaucoma in adults:
You’ll attend a pre-operative assessment – some simple tests will be done to check that you can have the operation and you’ll have the chance to ask any questions about it.
You’ll be told when to come into hospital for the procedure and when you should stop eating and drinking beforehand.
You’ll need to sort out how you’ll be getting home – you can usually go home the same day, ideally with a friend or family member to escort you (as you may be sleepy); you won’t be able to drive for at least a day or two if you’ve had surgery.
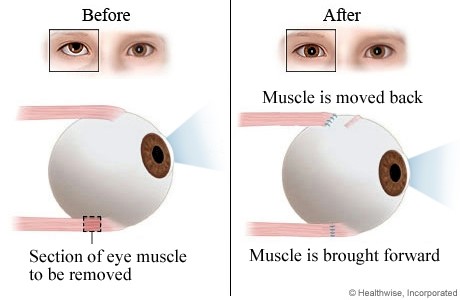
Squint surgery is done under general anaesthetic (where you’re asleep) and usually takes less than an hour. You or your child can usually go home the same day.
If your child is having surgery, you’ll be able to accompany them into the operating room and stay with them until they’ve been given the anaesthetic.
The eye is held open using an instrument called a lid speculum – sometimes it may be necessary to operate on both eyes to get the alignment right.
The surgeon detaches part of the muscle connected to the eye and moves it into a new position so that the eyes point in the same direction.
The muscles are fixed in their new position with dissolvable stitches – these are hidden behind the eye so you won’t be able to see them afterwards.
Sometimes, in adults and teenagers, further adjustments to your eye muscles may be made when you’ve woken up after the operation. Local anaesthetic eye drops are used to numb your eyes for this.
Following the operation, a pad may be put over the treated eye. This is usually removed the next day, or sometimes before you go home.
The eye is likely to be sore for at least a few days. You may be given painkillers to reduce discomfort and some eye drops to help with healing.
You may experience some of the following side effects:
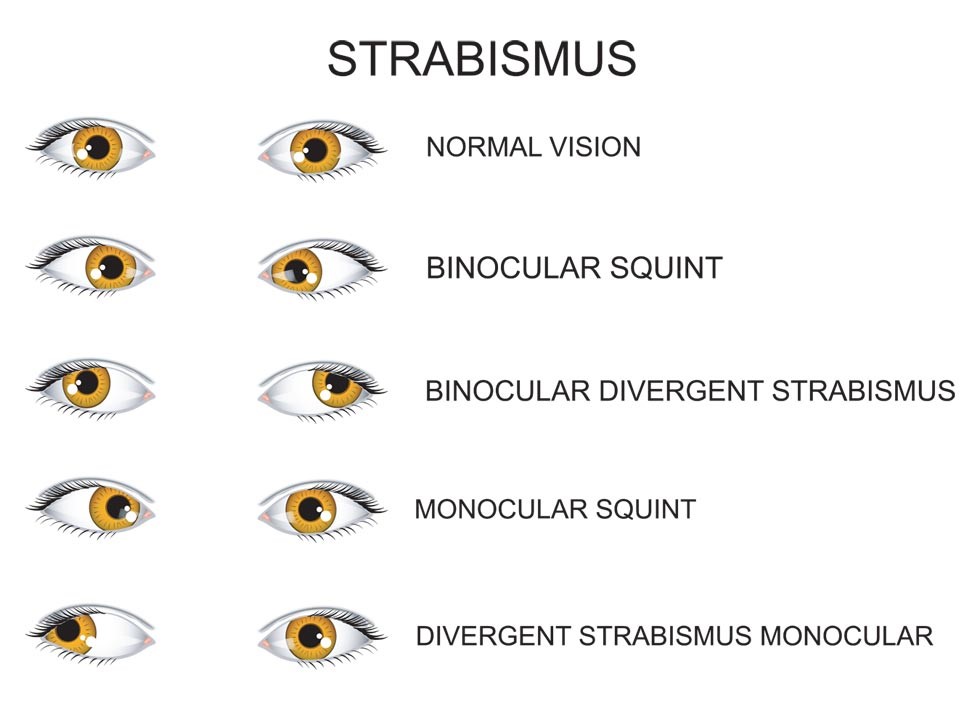
In adults, eye alignment surgery is not strictly cosmetic. Cosmetic surgery is enhancement surgery, such as restoring youthful appearance in a normal aging person. Eye alignment surgery restores normal appearance and is considered reconstructive. There are many other benefits beyond restoring normal appearance: improved depth perception or binocular vision, improved visual fields, eliminating or minimizing double vision and improved social function — as eye contact is hugely important in human communication. It is important to discuss the goals and expectations of the surgery with your ophthalmologist.
During strabismus surgery, one or more of the eye muscles are strengthened, weakened or moved to a different position to improve alignment. Strabismus surgery is usually performed as an outpatient procedure and does not require an overnight hospital stay.
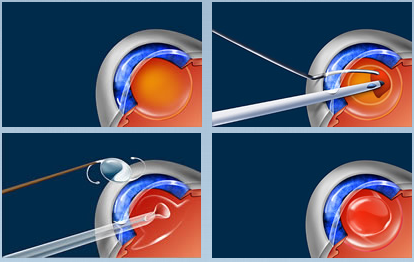
Vitrectomy is a surgery to remove the vitreous gel from the middle of the eye camera.gif. It may be done when there is a retinal detachment or if blood in the vitreous gel (vitreous haemorrhage) does not clear on its own. Removing the vitreous gel gives your eye doctor better access to the back of the eye. Vitrectomy is done by an eye doctor (ophthalmologist) who has special training in treating problems of the retina.
During surgery, the doctor uses small tools to remove the vitreous gel. Then the doctor may treat other eye problems, such as a retinal detachment, vitreous haemorrhage, scar tissue on the retina, or tears or holes in the macula.
At the end of the surgery, the doctor may inject an oil or gas bubble into the eye. This lightly presses the retina against the wall of the eye. If an oil bubble is used, the doctor will need to remove the oil after the eye has healed.

We offer a range of cutting-edge LASIK solutions to correct vision imperfections and improve your quality of life. Our advanced procedures include:
Silk Smile: Premium LASIK Solution
– Optimal Vision Correction: Our premium LASIK solution for achieving optimal vision correction
– Minimally Invasive: Blade-free technology for reduced risk and faster recovery
– Customized Treatment: Personalized to address unique vision needs
ICL (Implantable Collamer Lens): Minimally Invasive Alternative
– Implantable Lens: A flexible, biocompatible lens implanted inside the eye
– Minimally Invasive: Small incision, reducing risk and promoting faster healing
– Reversible: Can be removed if needed
Blade-Free LASER: Advanced Vision Correction
– Precise Correction: Advanced laser technology for precise vision correction
– Reduced Risk: Blade-free procedure minimizes risk of complications
– Faster Recovery: Quick healing time, getting you back to your routine sooner
Contoura: Personalized LASIK
– Unique Vision Needs: Customized treatment addressing specific vision imperfections
– Advanced Mapping: Detailed mapping of the eye’s surface for precise correction
– Optimal Results: Personalized approach ensures optimal vision correction results
WhatsApp us