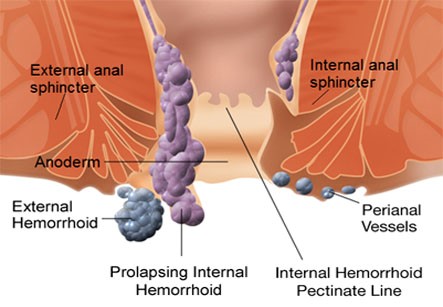
A hemorrhoidectomy is surgery to remove internal or external hemorrhoids that are extensive or severe. Surgical hemorrhoidectomy is the most effective treatment for hemorrhoids, though it is associated with the greatest rate of complications.
Inguinal hernia surgery is an operation to repair a weakness in the abdominal wall that abnormally allows abdominal contents to slip into a narrow tube called the inguinal canal in the groin region.
Surgery remains the ultimate treatment for all types of hernias as they will not get better on their own, however not all require immediate repair.Elective surgery is offered to most patients taking into account their level of pain, discomfort, degree of disruption in normal activity, as well as their overall level of health. Emergency surgery is typically reserved for patients with life-threatening complications of inguinal hernias such as incarceration and strangulation. Incarceration occurs when intra-abdominal fat or small intestine becomes stuck within the canal and cannot slide back into the abdominal cavity either on its own or with manual maneuvers. Left untreated, incarceration may progress to bowel strangulation as a result of restricted blood supply to the trapped segment of small intestine causing that portion to die. Successful outcomes of repair are usually measured via rates of hernia recurrence, pain and subsequent quality of life.
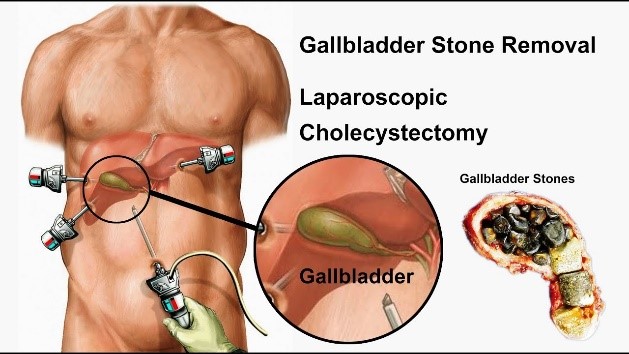
During a laparoscopic surgical procedure, small incisions of up to half an inch are made and plastic tubes called ports are placed through these incisions. The camera and the instruments are then introduced through the ports which allow access to the inside of the patient. The camera transmits an image of the organs inside the abdomen onto a television monitor. The surgeon is not able to see directly into the patient without the traditional large incision. The video camera becomes a surgeon’s eyes in laparoscopy surgery, since the surgeon uses the image from the video camera positioned inside the patient’s body to perform the procedure.
Benefits of minimally invasive or laparoscopic procedures include less post operative discomfort since the incisions are much smaller, quicker recovery times, shorter hospital stays, earlier return to full activities and much smaller scars. Furthermore, there may be less internal scarring when the procedures are performed in a minimally invasive fashion compared to standard open surgery.
Partial Colectomy is the removal of part of the large intestine (colon) which may be performed to treat cancer of the colon or long-term ulcerative colitis.
It is also known as Bowel resection in wihich doctors removes a diseased or damaged part of the colon or rectum. Bowel resection can be done for many diseases that affect the colon, such as colorectal cancer, diverticulitis, or Crohn’s disease.
The goal of bowel resection is to take out the part of the colon or rectum where the problem is. If the doctor is removing cancer from the colon, nearby lymph nodes are taken out and tested for cancer. Then healthy parts of the colon or rectum are sewn back together. Bowel resection is done either by opening the abdomen (open resection) or by laparoscopy. Bariatric Surgeries/ Weight loss surgery
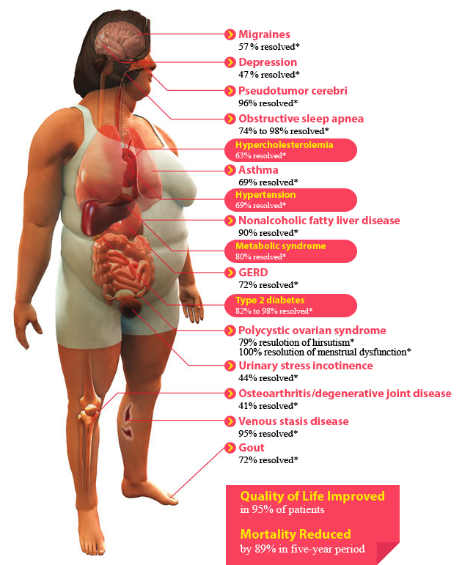
Weight-loss (bariatric) surgery helps you lose weight and lowers your risk of medical problems associated with obesity. Bariatric surgery contributes to weight loss in two main ways:
Four common types of weight loss surhery are:
In Roux-en-Y gastric bypass, the surgeon creates a small pouch at the top of the stomach. The pouch is the only part of the stomach that receives food. This greatly limits the amount that you can comfortably eat and drink at one time. The small intestine is then cut a short distance below the main stomach and connected to the new pouch. Food flows directly from the pouch into this part of the intestine. The main part of the stomach, however, continues to make digestive juices. The portion of the intestine still attached to the main stomach is reattached farther down. This allows the digestive juices to flow to the small intestine. Because food now bypasses a portion of the small intestine, fewer nutrients and calories are absorbed.
In the laparoscopic adjustable gastric banding procedure, a band containing an inflatable balloon is placed around the upper part of the stomach and fixed in place. This creates a small stomach pouch above the band with a very narrow opening to the rest of the stomach.
A port is then placed under the skin of the abdomen. A tube connects the port to the band. By injecting or removing fluid through the port, the balloon can be inflated or deflated to adjust the size of the band. Gastric banding restricts the amount of food that your stomach can hold, so you feel full sooner, but it doesn’t reduce the absorption of calories and nutrients.
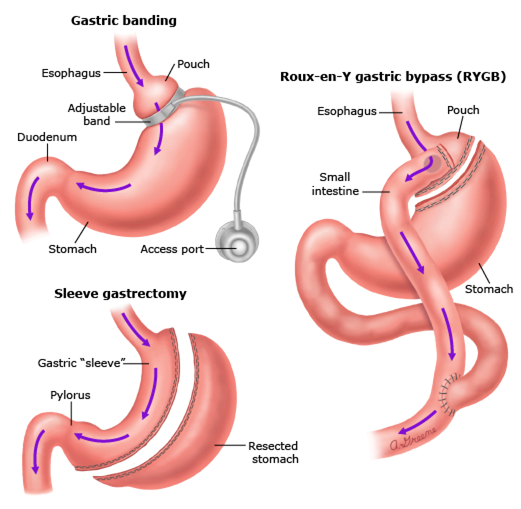

The surgeon then closes off the middle section of the intestine and attaches the last part directly to the duodenum. This is the duodenal switch.
The separated section of the intestine isn’t removed from the body. Instead, it’s reattached to the end of the intestine, allowing bile and pancreatic digestive juices to flow into this part of the intestine. This is the biliopancreatic diversion.
As a result of these changes, food bypasses most of the small intestine, limiting the absorption of calories and nutrients. This, together with the smaller size of the stomach, leads to weight loss.
WhatsApp us